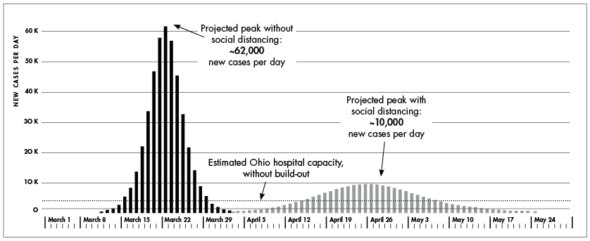
Ohio hospitals are preparing for a surge of patients with COVID-19. The curve to the left depicts the projected surge without social distancing measures; the curve on the right depicts a dampened curve with these measures in place. Even on the flattened curve, Ohio hospitals may need to double or possibly triple their bed capacity, particularly in the ICU, to care for patients with the illness, new modeling from the Cleveland Clinic predicts. Projections are current as of March 28. (Chart data from Ohio Department of Health)
Ohio hospitals prepare for surge
- Published: April 2, 2020
Hospital beds set up in convention centers. Surgeons redeployed as nursing staff. New technology to sterilize surgical masks for reuse. Whiskey distilleries manufacturing hand sanitizer.
Those are just a few of the plans and proposals underway in Ohio as hospitals prepare for a surge in COVID-19 cases that state officials say could be about two weeks away.
Hospitals have been working for months to prepare for the spread of COVID-19 to Ohio, but efforts have intensified over the past couple of weeks, as known cases have grown to over 2,000 and the state braces for an influx of patients sick with symptoms of the highly infectious respiratory illness.
Ohio could see as many as 10,000 new cases per day, new modeling from The Ohio State University predicts. Modelers estimate the peak will come around April 25. Most of those cases won’t be confirmed, as testing remains limited in the state, and most people infected with the new coronavirus won’t require hospitalization.
But about 20% of those with COVID-19 will land in the hospital, and about 11% of those will end up in the ICU, data from other states and countries and Ohio’s own experience shows. That caseload would quickly overwhelm Ohio’s healthcare system, as has been seen in New York City, the Lombardy region of Italy and elsewhere, Ohio Health Director Dr. Amy Acton has said.
“No hospital system in the world has ever faced what we’re facing now. Our planning will go through the surge and after the surge,” Acton said on Monday, referring to the overall pandemic.
Based on the new modeling, the Cleveland Clinic is predicting that Ohio hospital systems need to at least double, and maybe triple, their capacity to care for COVID-19 patients and people ill with other diseases. Doubling ICU capacity is especially urgent, because those critically ill with COVID-19 require intensive care, including ventilator support, delivered in that setting.
As Ohio prepares for the hospital surge, this article takes an overall look at the state’s hospital capacity, with specific information about capacity and planning in the Dayton area.
Ohio hospital capacity
Across the state, hospital capacity is at or under 60%, according to the most recent information from Gov. Mike DeWine’s daily press conferences. That means about 60% of hospital beds are filled, with about 40% of beds available for new patients.
That capacity level has dropped from 70% or more over the past couple of weeks as hospitals have postponed elective surgeries, complying with a state order effective March 18 to do so.
According to figures from the Ohio Health Department last week, Ohio has a total of 15,000 medical/surgical beds and 3,600 ICU beds. About 6,000 of the medical/surgical beds were available as of last week, and about 1,300 ICU beds were available.
How many beds hospitals will need to cope with a surge in patients depends on which predictive models are consulted. The Cleveland Clinic modeling, as mentioned above, suggests that hospitals will need to double or triple capacity, especially in the ICU.
By contrast, a new model from the Institute for Health Metrics and Evaluation, or IHME, a global research center at the University of Washington, predicts that Ohio won’t experience bed shortages on the projected peak date of the illness of April 21.
Public health modeling is highly complicated and relies on many factors, including the behavior of millions of individuals, explained Don Brannen, an epidemiologist with Greene County Public Health, reached for comment this week.
“We’re impacting the models by how we behave,” he said.
With so many assumptions built into highly theoretical models of a new disease, divergent predictions are inevitable, he said.
Yet another model, one from the Harvard Global Health Institute, which correlates hospital bed capacity and COVID-19 estimates, suggests that American hospitals will almost inevitably be overwhelmed, unless they build out additional bed capacity.
“Even in a best-case scenario, with cases of the coronavirus spread out over 18 months, American hospital beds would be about 95% full,” a March 17 report on the model by ProPublica states.
Ohio’s aggressive social distancing measures, including closing schools and nonessential businesses, canceling in-person voting and issuing a “stay-at-home” order, are all aimed at the “best case” — slowing the spread of disease and giving Ohio hospitals time to build out capacity.
“Social distancing is buying us time,” DeWine asserted at a recent press conference.
Eight-region planning model
To meet the anticipated surge, Ohio has been divided into eight regions, and each region recently submitted its plan for building bed capacity, deploying more healthcare workers and increasing medical equipment and supplies. Those plans are a working draft of how hospitals intend to respond, and what resources and support they will need from the state. Details about the regions and their plans have not yet been made publicly available.
To help hospitals and communities coordinate their response to COVID-19, Ohio has tapped the Ohio National Guard, under the command of Gen. John Harris.
“We are turning over every rock possible,” Harris said on Monday, noting that National Guard servicemembers will become visible in communities as they support the hospital effort.
In the coming days and weeks, Ohio hospitals will be expanding capacity by coordinating in unprecedented ways, not only with each other, but also with community partners such as nursing homes and long-term care units, as well as hotels, convention centers and colleges and universities. Any one of those sites could be converted into a hospital setting to accommodate noninfectious patients while hospitals themselves care for those critically ill with COVID-19.
Of course, bed capacity is just part of the story. According to Acton during recent press conferences, Ohio is also scaling up its healthcare workforce by redeploying existing and retired workers, expediting jobs for medical students near the end of their training and extending or waiving licensure renewals for nurses.
As is true of other states, Ohio is facing critical shortages of personal protective equipment, or PPE, such as gloves, gowns, surgical masks and face shields. All are needed to protect healthcare workers, first responders and people in nursing homes and long-term care settings from becoming infected by the coronavirus.
Ohio has received its total allotment of PPE from the national stockpile, but that amount was far short of what the state needs. Gov. DeWine and other officials have described a variety of efforts to increase PPE, most recently including a new technology coming available from Columbus-based Battelle that is sterilizing N95 masks for reuse, conserving the highly protective surgical masks.
Ohio hospitals will also need to scale up their supplies of ventilators, a breathing-support machine essential to treating patients with life-threatening respiratory symptoms.
A recent graph from the Ohio Department of Health shows that about 30% of ventilators in the state are being used, with 70% availability. But officials are not yet saying how large that overall supply of ventilators is. A widely reported 2010 study published by Cambridge University estimates that the U.S. at that time had 62,188 full-feature ventilators and Ohio had 2,729.
On Tuesday, Ohio Public Health Director Acton issued an order requiring weekly online reporting of these devices, a step toward their identification and redistribution.
Ohio officials have said that hospitals are working to adapt their ventilators to allow multiple patients to be hooked into a single unit, and they are seeking more ventilator tubing material to permit that modification.
Dayton area planning
Dayton area hospitals have yet to see a surge of COVID-19 patients, according to Sarah Hackenbracht, president and CEO of the Greater Dayton Area Hospital Association, or GDAHA. The association is a member organization for 29 hospitals and medical centers in 11 counties, including Greene, Clark, Montgomery and Miami.
“We are seeing an increase in patient volume, but we are not yet to a surge in our area,” Hackenbracht said this week.
But with known COVID-19 cases growing locally, including 37 known cases in Montgomery County, six in Greene County and six in Clark County, area hospitals are preparing for the surge, expected here within two to three weeks.
Most of the hospitals in the GDAHA are included in region 3 of Ohio’s eight-region planning model, according to Hackenbracht. Those hospitals submitted a draft plan to the Ohio Department of Health on Saturday, and continue to refine the plan based on feedback from government and health department planners. While specific details are not yet publicly available, one focus of the plan is to double ICU capacity in the region, Hackenbracht said.
Different hospitals are doing this in different ways, some by converting their existing facilities to ICU settings, while working with community partners such as nursing homes or hotels to convert those spaces to hospital settings for noninfectious patients.
“There are a range of approaches,” she said.
Another focus of the plan is to respond to the Dayton area surge within the region. While patients and resources could be moved throughout the state and even across state lines, depending on the intensity of the surge, the goal with regional planning is to treat the local community within the region as much as possible.
“Our goal as a local healthcare community is to care for as many people as possible locally,” Hackenbracht said.
Hackenbracht declined to release the total number of medical/surgical beds, ICU beds or ventilators currently within the Dayton region. However, regarding bed number, the recent ProPublica report on the Harvard Global Health Institute model indicates that the Dayton region as of 2018 had 2,070 hospital beds and 290 ICU beds, with a little over 60% occupancy.
Based on those numbers and the researchers’ surge model, Dayton “would be among the regions that would need to expand capacity,” the ProPublica report states.
Within Greene County, there are two hospitals, Soin Medical Center and Greene Memorial Hospital, both part of the Kettering Health Network. A Kettering spokesperson declined to specify current bed counts, but Ohio hospital registration data from 2018 shows that Soin had 101 medical/surgical beds and 12 ICU beds, and Greene Memorial had 41 medical/surgical beds and eight ICU beds.
In February, Greene Memorial Hospital announced that it was closing its ICU because the doctor group operating the unit had pulled out. However, in response to a question from the News last week, the Kettering spokesperson said the intensive care unit was back online.
“The Greene Memorial ICU beds are online and ready to use in the event of a surge in patient volume,” the spokesperson wrote in an email.
Strong regional preparedness
As Dayton area hospitals plan for a COVID-19 surge, they are building on 20 years of emergency preparedness and pandemic planning that began after 9/11, according to Hackenbracht.
“Groundwork and preparedness is very, very strong in our region,” she said.
As recently as Feb. 11, Dayton area hospitals took part in a pandemic flu exercise. Such exercises involve virtual scenarios where hospitals are required to (virtually) evacuate patients to other facilities, as well as other tabletop exercises involving moving critical resources across facilities.
Since 2003, Dayton area hospitals have reported and shared bed availability through an online platform called Surgenet. Hospitals are also now reporting and sharing PPE availability through that platform.
And a data modeling group affiliated with the GDAHA is working to apply various predictive models of COVID-19 to the Dayton area. Hackenbracht said the local region has a few unique features, including nearly 80% of people on Medicare or Medicaid. Older and more medically vulnerable people are at higher risk for COVID-19, medical authorities say.
Collaboration and coordination is already strong among Dayton area medical systems, according to Hackenbracht. But the COVID-19 pandemic will turn testing exercises and shared platforms into urgent real-life situations, she acknowledged.
“We’ve never seen this pandemic before. This is where our planning really gets tested,” she said.
The Yellow Springs News encourages respectful discussion of this article.
You must login to post a comment.
Don't have a login? Register for a free YSNews.com account.










No comments yet for this article.